 Introduction:
Introduction:
Urodynamics (UDS) is an interactive diagnostic study of lower urinary tract function. It is composed of several tests that can be used to obtain functional information about urine storage and expulsion. Its main goal is to reproduce the patients’ symptoms and determine their cause.
The present article is a review of the physiological concepts behind UDS, and explains the various normal and abnormal forces and parameters that are measured and used during the tests to assist the physician in making a diagnosis. It outlines the importance and methods of the calibration of UDS equipment to optimize diagnostic accuracy and reliability, which would have a crucial impact over the treatment’s decision, and consequently the patient’s outcome.
Physiological Background of UDS
The concept of all pressure measurements in UDS is that pressure is related to a force acting perpendicular to a surface within a fluid medium. There is no direction assigned to the pressure measurement since even when the surface is twisted around, the direction may change but there is no change in the magnitude of the force. There are four types of pressures that are important to determine the influence of the forces on LUT:
Intravesicular Pressure (Pves)
Considering variations of pressure within the bladder, ICS has established the superior margin of the symphysis pubis as the reference point for measuring all UDS pressures. For unreliable cases, consider the level of transducer itself as the reference level for pressure measurement.
Abdominal Pressure (Pabd)
These are the pressures exerted by the abdominal and thoracic structures at rest (passive pressures) and during active forces like physical exertion, coughing, sneezing (active pressures), Pabd helps the urodynamic clinician to differentiate the effects of abdominal from detrusor forces. Pabd is only relative and cannot be estimated accurately in a clinical setting and is vulnerable to many physiological artifacts.
Detrusor Pressure (Pdet)
It is created by the tone of smooth muscle within the bladder wall and passive forcers exerted by the viscoelastic properties of the bladder wall. Pdet can be calculated as Pdet = Pves – Pabd. It is also a relative pressure prone to physiological artifacts.
Getting Started: Transducers, Zeroing-to-Air, and Equipment Calibration
Pressures Transducers
When using water-filled (external) transducers, the ICS Reference is at the level of the pubis symphysis, should be filled with fluid and the connection tubing exposed to known pressure by raising the fluid-filled line about 50–100 cm above the level of transducer reservoir. A common source of artifact in this type of transducers is air bubbles in connection tubing.
Microtransducers - ICS Reference is at the level of the transducer within the LUT, bowel, or posterior vaginal vault
Fibreoptic sensor transducers - should be used as the microtranducers and are calibrated automatically before UDS measurement.
Air charged catheters - the air-charged sphere is lowered into a graduated beaker or cylinder (10–25 cm) to generate a known pressure. A specialised pressure chamber made by the transducer manufacturer (Wilmington, USA, DE, T-Doc) also may be used for calibration.
Zeroing to Air
Once the filling catheter, vesical transducer and rectal transducer lines are in position, the latter two are connected to their respective transducer domes. Zeroing to the pressure of atmosphere is done and the patient is asked to cough to check for accuracy. Once done, cystometry can begin. Initially fill the bladder with a small volume of fluid to prevent inaccurate subtraction and false readings.
Routinely all three pressures, Pves, Pabd, Pdet are measured. First during early bladder filing. Record multiple times for accuracy.
Pelvic Floor Electromyography (EMG)
Performed for striated muscles of perineum to look for abnormalities and detect if their contractions are coordinated or uncoordinated with detrusor with surface electrodes or concentric needle electrodes. The biggest drawback of EMG is that it is nonspecific and technically challenging.
Maintenance of Equipment and Calibration
The calibration of UDS equipment should be applied on a regular basis to the transducers, flowmeter, and infusion pump if used, with attention to the manufacturer’s recommendation. Calibrations should include zero balancing, amplitude adjustments, flowmeter calibration, and pump calibration (by using an accurate volume at a constant flow into the flowmeter, roughly 400 mL in 20–30s at 15–20 mL/s and checking the recorded volume).
Artifacts
Physiological Artifacts
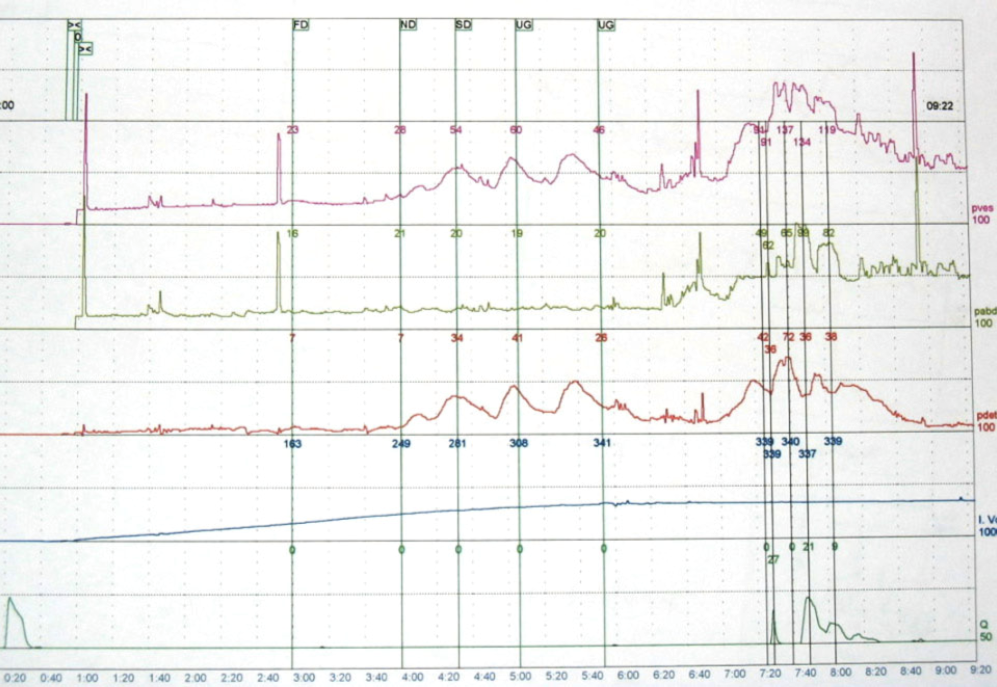
Show normal trace with good subtraction (Figure 1). This type of artifact occurs when an anticipated physiological event occurs that transiently changes the accuracy of pressure measurements. For instance, artifacts associated with rectal vault contraction during the test.
Figure 1
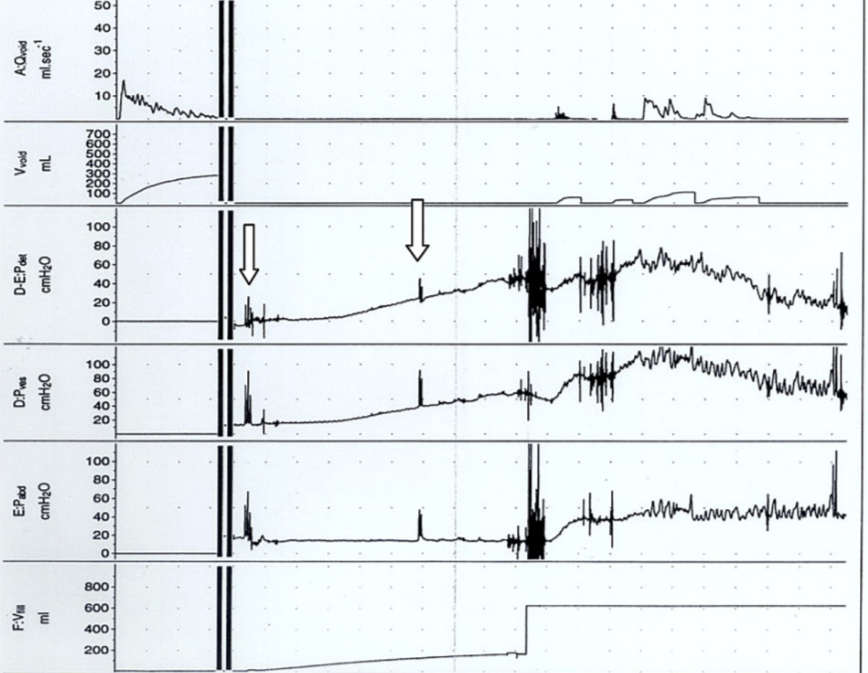
A transient drop in Pabd, often seen as gas, can be expelled from the rectum during coughing or Valsalva causing a small corresponding rise in Pdet created by subtracting negative numbers. This physiological artifact can be easily confused with a ‘cough induced’ detrusor contraction by the uninformed eye (Figure 2).
Figure 2
Technical Artifacts
- Presence of a kink or gas bubbles in the tubings of water filled transducers.
- Connection of the Pves and Pabd lines to the wrong transducer domes.
- Mucosal seal effects when the Pves abuts the bladder mucosa in an empty bladder initially.
- Dampening or stepping of lines from partial blockage from anaesthetic gel or blood clots from Pves line dislodging gradually out of the bladder.
Other Caveats
- There should be ample length of the Pves line inserted into the bladder lumen, especially in patients who are likely to have high-pressure obstruction, to prevent dislodgement of the line during voiding
- Maximal silencing of an EMG trace requires adjacent electrical appliances to be switched off.
- Commands may need to be in simple terms and spoken clearly and slowly in the elderly to gather a really accurate interpretation of the urodynamic findings.
Conclusion
UDS is an essential investigation that can assist in the diagnosis of LUT dysfunction. The test aids in management and for checking treatment progress. For best usage and interpretation of the test, it is of utmost importance that the physician be present during the test, be aware of methodology in effectively zeroing the system to air before filling. Most importantly, it’s essential to be aware of visual cues and feedback by the patient during the study, to ensure regular calibration and maintenance of equipment, as well as being cognisant of artifacts that may occur.
If you would like to perform urodynamic testing in your practice without buying equipment or having to train staff, click on the button below.


