When evaluating patients prior to surgery for the treatment of stress urinary incontinence, the presence of detrusor overactivity is presently the main factor that is tested for via urodynamics, if urodynamic assessment happens at all. However, there are numerous factors which could influence the diagnosis of stress urinary incontinence, as well as the surgical procedure and predictions for the outcome of treatment.
In a 2016 article published in Journal of Mid-Life Health1, researchers from India questioned the present role of urodynamics in the treatment of stress urinary incontinence, and suggested that urodynamic evaluation should play a more prominent role in preoperative consultation.
Besides detrusor overactivity, the presence of voiding inefficiency, asymptomatic detrusor overactivity, and severity of stress urinary incontinence should be considered. The hypothesis of the paper’s authors was that the aforementioned factors can hinder the evaluation of patients exhibiting symptoms of stress urinary incontinence, and the main objective of this study was to analyze the overall voiding dynamics of patients suffering from lower urinary tract symptoms via urodynamics, in conjunction with clinical findings. The results from this study will be comprehensively summarized here.
Do you need to begin offering urodynamics testing in your practice? If so, click the button below.
Introduction
Stress urinary incontinence is a highly prevalent occurrence among women (affecting up to 35%2 of the population), yet surgical outcomes are unpredictable. The lower urinary tract system is complex, which further complicates diagnosis and treatment.
A frustrating aspect for both physicians and patients is that surgical procedures can sometimes cure the issue entirely; while in other instances they can make matters worse. For the best surgical results, positive identification of the underlying cause of stress urinary incontinence is crucial.
At present, the primary manner in which stress urinary incontinence is diagnosed is via positive identification of symptomatic or asymptomatic detrusor overactivity. However, in the search for detrusor overactivity, many other important variables are ignored.
These factors include detrusor underactivity, bladder outlet obstruction, pelvic organ prolapse, and degree of stress urinary incontinence severity. The authors of this study believe that preoperative evaluation that takes all of these factors into consideration will improve surgical outcomes.
The main objective of this study, entitled Role of Urodynamics in Stress Urinary Incontinence: A Critical Appraisal was to utilize urodynamics for better identifying and quantifying underlying disorders in female patients exhibiting symptoms of stress urinary incontinence.
The findings were correlated with data obtained through clinical evaluation, such as a full urodynamics work up. The value of urodynamics for preoperative patients suffering from stress urinary incontinence will be critically evaluated.
Methods and Materials
This study utilized 100 patients who had been referred to the clinic for urodynamic evaluation of stress urinary incontinence between February 2013 and January 2015. The International Consultation on Incontinence Questionnaire3 was used for screening.
Read more about Urodynamics Incontinence Screening Questionnaires
A physical exam was performed and the patient’s detailed medical history was provided. Included in the physical was pelvic exam, measurement of pelvic floor strength, urinary stress test, as well as neurological assessment for sacral reflex arc.
An ultra sound of the urinary tract was performed, and urine was tested for possible presence of urinary tract infection. The voiding patterns of participants were also acquired.
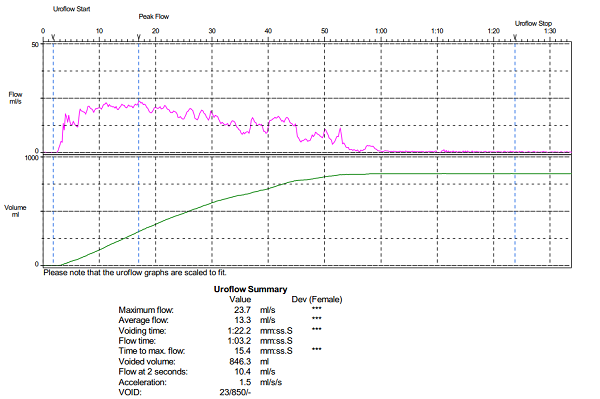
For urodynamic studies of flow rate, multichannel cystometry, residual urine volume measurement, leak point pressure, Valsalva maneuver, and pressure flow studies, the standards of Good Urodynamics Practices4 were followed.
Results
Out of the 100 patients that had previously described symptoms of stress urinary incontinence, 49 study participants reported urinary storage symptoms, such as increased urinary frequency and / or urgency, while 51 patients did not report such symptoms. As shown in Table 1, urodynamic tests found that 23 patients of the initial 49 who reported storage symptoms tested positive for detrusor overactivity.
In comparison, 26 women showed no indication of detrusor overactivity. Additionally, of the 51 patients that did not have associated storage symptoms, urodynamic assessment indicated 15 of these women had detrusor overactivity, while the remaining 36 did not.
Ultimately, there was no statistically significant correlation between urodynamic findings of urinary frequency, urgency, and detrusor overactivity, meaning that simply taking a patient’s clinical history is not a reliable method for diagnosing stress urinary incontinence.
Correlations were also made between reported symptoms of urge incontinence with clinical findings of detrusor overactivity, which is shown in Table 2. Overall, 31 patients reported stress urinary incontinence symptoms of urge incontinence, but during urodynamic assessment only 23 patients displayed characteristics of detrusor overactivity.
The remaining 8 study participants did not. Among the other 69 women that did not report symptoms of urge incontinence, 15 patients were clinically shown to have detrusor overactivity, while 54 showed no symptoms of this disorder. These correlations are statistically significant, which suggests that the presence of urge incontinence in a patient can reliably be used as a predictor for detrusor overactivity.
However, detrusor overactivity is not the only reason that a patient might experience symptoms of urge incontinence. Sphincter deficiency was also tested, which was defined to occur at an abdominal leak point pressure <60 cm water. As shown in Table 3, of the 31 patients that initially reported symptoms of urge incontinence, 8 women displayed sphincter deficiency, while 23 patients did not.
On the other hand, of the 69 participants that reported no symptoms of urge incontinence, 4 patients displayed intrinsic sphincter deficiency, while the remaining 65 patients showed no symptoms of this disorder. This result shows that is important for clinicians to consider there may be multiple underlying causes behind a patient’s symptoms when counseling a preoperative patient with stress urinary incontinence.
As shown in Table 4, which correlates the occurrence of asymptomatic detrusor overactivity with storage symptoms, of the 51% of patients that did not report storage symptoms, 15 women had detrusor overactivity, as indicated by urodynamic assessment. Therefore, clinicians should beware that patients reporting an absence of storage symptoms does not rule out detrusor overactivity.
Additionally, this study suggests that asymptomatic detrusor overactivity could be a prevalent problem, affecting up to 15% of patients with symptoms of stress urinary incontinence.
Next, voiding dysfunction was compared with urodynamic findings. Out of the study’s 100 participants, 53 reported symptoms of voiding dysfunction. However, as shown in Table 5, only 25 patients tested positive for detrusor underactivity and/or bladder outlet obstruction, while 28 patients showed no symptoms of these disorders.
Additionally, of the 47 patients that did not express symptoms of voiding dysfunction, 15 study participants were verified via urodynamics to have detrusor underactivity and /or bladder outlet obstruction. The correlation between patients who self-reported symptoms voiding dysfunction and the urodynamic findings of bladder outlet obstruction or detrusor dysfunction are not statistically significant, which shows that physicians should not solely rely on clinical information for the prediction of voiding dysfunction.
Table 6 shows the percentage of patients that have voiding dysfunction and the correlating urodynamic findings of detrusor underactivity (as opposed to bladder outlet obstruction). Of the 53 patients that had symptoms of voiding dysfunction, 18 had urodynamic findings of detrusor underactivity alone, while 35 did not.
Of the 47 participants who did not express symptoms of voiding dysfunction, 25 were found to have detrusor underactivity alone, while 22 were not show signs of this disorder. Therefore, there is not a statistically significant correlation between detrusor underactivity, as diagnosed via urodynamics, and reported symptoms of voiding dysfunction.
Finally, Table 7 correlates reported symptoms of voiding dysfunction with urodynamic findings of bladder outlet obstruction alone, without the incidence of detrusor underactivity. Of the 53 participants reporting voiding dysfunction, 22 tested positive for bladder outlet obstruction, while 31 women did not have indications for BOO. Of the 47 participants who did not report voiding dysfunction, 24 women had urodynamic findings of bladder outlet obstruction, while the other 23 participants did not.
There is no statistically significant correlation between bladder outlet obstruction and symptoms of voiding dysfunction in this study, meaning that clinical findings of bladder outlet obstruction do not predict symptoms of voiding dysfunction.
The results discussed in Table 6 and Table 7 shows that voiding dysfunction cannot be diagnosed solely by the patient’s discussion of symptoms. Instead, urodynamic studies should be performed in order to verify the presence or absence of lower urinary tract abnormalities. Urodynamic studies are important because they also have the ability to distinguish between detrusor underactivity and bladder outlet obstruction, which aids in the diagnosis and treatment of the voiding dysfunction.
Discussion
In this article, the authors assert that the usefulness of preoperative urodynamic evaluation for cases of stress urinary incontinence management is highly debated. In fact, the vast majority of studies on this topic conclude that urodynamic evaluation does not add clarity to the surgical proceedings in most situations.
However, the two instances where urodynamics are recommended as a preoperative measure are when previous surgical interventions have failed, and when there is reason to believe that detrusor overactivity is the underlying cause of urge incontinence.
In fact, most clinical studies have highlighted the need for diagnosing detrusor overactivity5 in cases of stress urinary incontinence. Indeed, the most comprehensive diagnosis of associated and underlying disorders requires analysis of the entire lower urinary tract. In particular, data regarding voiding inefficiency and detrusor contractility are important, and should influence the manner in which physicians choose appropriate treatments for their patients.
From a practical perspective, there are numerous challenges6 to the management of stress urinary incontinence. These include the presence of voiding dysfunctions, bladder outlet obstruction, incomplete clinical evaluation, variation of symptoms relative to severity of incontinence, and the presence of mixed symptoms as a result of detrusor overactivity.
The 100 women that participated in this study presented to the department with symptomatic stress urinary incontinence, and were mainly referred to the study for preoperative evaluation. The main objective of this study was to determine various factors of voiding dysfunction in women experiencing stress urinary incontinence.
In general, the clinical information commonly utilized for the diagnosis of stress urinary incontinence in women includes full medical history, a physical examination, urine frequency and volume charts, and uroflowmetry. In addition, factors such as the magnitude of leakage, the presence of detrusor underactivity, and the presence of a bladder outlet obstruction can also be used in the diagnosis of stress urinary incontinence.
Here, the authors of this study attempted to compare each of these factors with urodynamic parameters. For each of the 100 patients complaining of stress urinary incontinence symptoms, the exact role of urodynamics for the group of patients was determined.
As indicated in Table 1, there is no correlation between symptoms of increased urinary frequency and urgency (with or without incontinence) with detrusor overactivity. Therefore, physicians should not jump to the conclusion of detrusor overactivity when only evaluating a patient’s symptoms. Additional studies7 by other authors have also verified this result.
However, the diagnosis of detrusor overactivity can be made more reliably when urge incontinence is the predominant symptom that a woman experiencing stress urinary incontinence expresses. This data is presented in Table 2, where a statistical correlation between urge incontinence and urodynamic observation of detrusor overactivity was recorded. Therefore, for patients that complain of the of urge incontinence as their primary symptom, a detrusor overactivity diagnosis can be made more reliably. This finding was corroborated in in a similar study8.
On the other hand, for certain patients that reported urge incontinence as the primary symptom, the absence of detrusor overactivity was noted. For these patients, intrinsic sphincter deficiency (defined as abdominal leak point pressure <60 cm water during Valsalva maneurver) was observed. Therefore, physicians should be aware that patients can show symptoms of severe stress urinary incontinence, when in reality the underlying cause of their disorder is related to sphincter deficiency.
As indicated in Table 3, severe intrinsic sphincter deficiency can be reliably predicted by careful consideration of the patient’s symptoms. However, in order to differentiate whether the patient is suffering from symptoms of urge incontinence due to detrusor overactivity or intrinsic sphincter deficiency a more thorough urodynamic examination is required. Similar studies have also correlated these findings9.
For women that exhibit symptomatic detrusor overactivity following surgery for stress urinary incontinence, it is very likely that they suffered from asymptomatic detrusor overactivity preoperatively. Therefore, women that do not report associated symptoms with detrusor overactivity could still benefit from urological assessment. An additional study with similar findings can be found here10.
Moreover, the results indicated in Table 4 show that no correlation with statistical significance for patients that are asymptomatic for storage symptoms yet have detrusor overactivity as verified by urodynamics. For women that do not complain of symptoms such as urinary urgency, frequency, or urge incontinence, detrusor overactivity should not be ruled out as a cause for their disorder. Likewise, this assertion is supported by additional research11.
In this study, 53 of 100 women had associated voiding symptoms of stress urinary incontinence. The primary symptoms were straining, hesitancy, and weak urine stream. Of those 53 patients, 25 were found to have significant detrusor underactivity, bladder outlet obstruction, or a combination of the two.
Of the 25 women with detrusor underactivity, bladder outlet obstruction, or a combination of these two factors, 18 had impaired detrusor contractility (data shown in Table 6). The remaining 7 women suffered from bladder outlet obstruction. This finding is significant because it suggests that physicians can improve their ability to predict potential postoperative problems, such as voiding difficulties and urine retention, by making this differentiation.
For these patients, preoperative counseling is useful, and should only be completed following a comprehensive urodynamic assessment. Women that were found to suffer from underactive detrusor should not be diagnosed solely via clinical examination and their medical history. While the discussion of symptoms is useful in the diagnosis of bladder outlet obstruction, urodynamic assessment is crucial for proper differentiation. This assertion is backed by Wang and Chen12 who found similar results.
The authors of this study underscore the importance of urodynamic assessment in the aforementioned instance, because the choice of surgical technique will be dependent upon whether the patient is suffering from bladder outlet obstruction or detrusor underactivity. If the inappropriate technique is chosen, a common side effect is urinary retention13.
Ultimately, it is the opinion of the authors that a properly conducted urodynamic evaluation will provide greater information regarding the patient’s voiding dynamics, which can result in a more informed surgical plan and better surgical outcomes.
Conclusions
Throughout this study, the authors have concluded that storage symptoms such as urgency and frequency (with or without urge incontinence) are not reliable predictors of detrusor overactivity. For women whose primary symptom is urge incontinence, however, detrusor overactivity can be more reliably diagnosed without additional clinical evaluation.
For women with voiding dysfunction caused by bladder outlet obstruction and / or an underactive detrusor, a diagnosis cannot reliably be made on the patient’s medical history alone. Instead, urodynamic assessment is necessary in order to differentiate between these two disorders and develop a surgical plan for the best outcome.
During this study, asymptomatic detrusor overactivity was observed among numerous patients in this group. These findings suggest that urodynamic evaluation and subsequent counseling are essential for any woman undergoing an invasive procedure to remedy the symptoms of stress urinary incontinence.
For some women, severe stress urinary incontinence, as diagnosed by low leak point pressure, can be mistaken for urge incontinence. In these cases, surgical intervention without proper diagnosis would likely limit the outcomes of the operation.
Overall, complete urodynamic evaluation can provide useful information regarding a woman’s voiding dynamics and leakage issues. A simple diagnosis of detrusor overactivity based on discussion of symptoms with the patient has been shown to have limited usefulness. Ultimately, urodynamic assessment provides a more precise and thorough preoperative evaluation, and results in better patient care.
Do you need help with staffing your urodynamics lab? If so, click the button below.
References
- Yande, S. D., Joglekar, O. V., & Joshi, M. (2016). Role of urodynamics in stress urinary incontinence: A critical appraisal. Journal of Mid-Life Health, 7(3), 119–125. http://doi.org/10.4103/0976-7800.191016 Link
- Luber, K. M. (2004). The Definition, Prevalence, and Risk Factors for Stress Urinary Incontinence. Reviews in Urology, 6(Suppl 3), S3–S9. Link
- Cotterill, N., & Abrams, P. (2010). International Consultation on Incontinence Modular Questionnaire (ICIQ). Textbook of Female Urology and Urogynecology, Third Edition, 138-145. doi:10.3109/9781439807217-19 Link
- Schäfer, W., Abrams, P., Liao, L., Mattiasson, A., Pesce, F., Spangberg, A., . . . Kerrebroeck, P. V. (2002). Good urodynamic practices: Uroflowmetry, filling cystometry, and pressure-flow studies**. Neurourology and Urodynamics, 21(3), 261-274. doi:10.1002/nau.10066 Link
- Sand, P. K., Hill, R. C., & Ostergard, D. R. (1987, July). Supine urethroscopic and standing cystometry as screening methods for the detection of detrusor instability. Retrieved May 24, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/3601269 Link
- Sivanesan, K. (2012, November 05). Urodynamics prior to surgery for urinary stress incontinence. Retrieved May 24, 2017, from http://sljog.sljol.info/articles/abstract/10.4038/sljog.v34i3.4887/ Link
- Wein, A. J. (2015). Clinical Risk Factors and Urodynamic Predictors prior to Surgical Treatment for Stress Urinary Incontinence: A Narrative Review. The Journal of Urology, 194(5), 1352. doi:10.1016/j.juro.2015.08.067 Link
- Ouslander, J., Staskin, D., Raz, S., Su, H. L., & Hepps, K. (1987, January). Clinical versus urodynamic diagnosis in an incontinent geriatric female population. Retrieved May 24, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/3795368 Link
- Ward, R. M., Hampton, B. S., Blume, J. D., Sung, V. W., Rardin, C. R., & Myers, D. L. (2008). The impact of multichannel urodynamics upon treatment recommendations for female urinary incontinence. International Urogynecology Journal, 19(9), 1235-1241. doi:10.1007/s00192-008-0610-2 Link
- Alperin, M., Abrahams-Gessel, S., & Wakamatsu, M. M. (2008). Development of de novo urge incontinence in women post sling: The role of preoperative urodynamics in assessing the risk. Neurourology and Urodynamics, 27(5), 407-411. doi:10.1002/nau.20526 Link
- Byrne, D. J., Stewart, P. A., & Gray, B. K. (1987, March). The role of urodynamics in female urinary stress incontinence. Retrieved May 24, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/3567483 Link
- Wang, A., & Chen, M. (2003). The correlation between preoperative voiding mechanism and surgical outcome of the tension-free vaginal tape procedure, with reference to quality of life. BJU International, 91(6), 502-506. doi:10.1046/j.1464-410x.2003.04130.x Link
- Jensen, J. K., Nielsen, J. R., & Ostergard, D. R. (1994, May). The role of patient history in the diagnosis of urinary incontinence. Retrieved May 24, 2017, from https://www.ncbi.nlm.nih.gov/pubmed/8159393 Link



