 Bladder management is a hugely important factor that needs to be taken into consideration when it comes to managing patients with spinal cord injury (SCI). In the following blog post, we will discuss differences between ambulatory urodynamics and conventional urodynamics on patients with SCI.
Bladder management is a hugely important factor that needs to be taken into consideration when it comes to managing patients with spinal cord injury (SCI). In the following blog post, we will discuss differences between ambulatory urodynamics and conventional urodynamics on patients with SCI.
According to this article1, conventional urodynamic testing has multiple drawbacks mainly due to the unfamiliar circumstances for the individual, immovability of the instrument, expenses, restrictive position during the test as well as manual filling of the bladder (rather than natural filling). Therefore, fully ambulatory urodynamic monitoring systems have been developed, which enable the pressure in the abdomen to be measured in a perfectly non-invasive manner. The question is: how reliable are they and can we use the findings effectively?
Contrasting Findings
Many clinicians actually question the usefulness of ambulatory urodynamics compared to standard urodynamics. A group from Switzerland2 conducted research on 33 men and 22 women with neurogenic lower urinary tract dysfunction due to acute SCI, finding that both ambulatory and nonambulatory patients have a similar risk of unfavourable urodynamic measurements. The physicians strongly recommend the same neuro-urological assessment including urodynamic investigations in all acute SPI patients independent of the ability to walk.
Similarly, a group of physicians from The Netherlands3 focused on the same issue. They found that ambulatory urodynamics don't seem to be necessary for risk assessment and diagnosis in SCI patients suspected of detrusor overactivity (DO) when conventional urodynamics are done properly. However, traditional urodynamics still had a high sensitivity and specificity and should not be excluded if there is no sign of DO.
A Big Advantage of Ambulatory Urodynamics
In patients with spinal cord injury, bladder management is of paramount importance, given the high risk of bladder stones, upper tract deterioration, urinary tract infections or incontinence. Urodynamic testing is an essential part of the routine follow-up of such patients and is frequently used to diagnose high-pressure storage, poor compliance or detrusor overactivity (DO), all of which can cause complications. Many physicians argue that traditional urodynamic testing is artificial, with the bladder being filled too fast in a situation where the patient is immobile. While this is not physiologically normal, a conventional urodynamic testing procedure lasts less than twenty minutes, and offers a quick snapshot of the lower urinary tract function.
The main difference between ambulatory urodynamics and traditional urodynamics is the prolonged period of time (usually a couple of hours) in the case of the former, during which the individual performs their typical daily activities. In other words, bladder filling is done with the individual's own urine production, so no other fluid is pumped in with the use of a catheter.
Key Studies
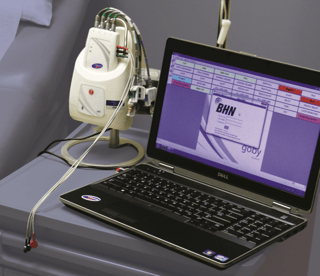
In this study1, Kim et al describe how they developed an ambulatory urodynamics monitoring system that uses a PDA to collect data. In their research, the physicians tested the device in twenty eight patients with SCI and compared their findings to traditional urodynamic procedures. What's really unique here is the fact that their device measures abdominal pressure using surface EMG patches. Plus, the system alerts itself to leakage by means of impedance changes in two sensors on the urethral catheter.
The measures are stored along with the bladder and rectal pressures and analyzed in the PDA. In the findings, researchers show that the rate of DO was actually higher when using ambulatory urodynamics than conventional urodynamics (60.7% vs 32.1%). Study limitations: all patients underwent the "ambulatory" urodynamics testing while in their hospital bed, and all of them had a filling cystogram performed before enrolling, which possibly resulted in bladder irritation from undergoing procedures in the same day. The result? A possibly elevated rate of DO which was observed in the second test. Concluding, researchers wrote that the ambulatory urodynamics system could be useful when traditional urodynamics fail to provide a diagnosis.
In another study3 published in Neurourology and Urodynamics, researchers discuss a study which includes 27 patients with spinal cord injury who went through ambulatory and traditional urodynamic procedures on the same day. They also concluded that although traditional urodynamic procedures might underdiagnose DO in a number of patients (a minority), a decent clinical assessment of the patient combined with conventional procedures is enough to make an accurate diagnosis of DO in individuals with SCI.
Conclusion
The results of the several studies performed on ambulatory urodynamics confirm what many physicians already believe. The substantial bother correlated with using bladder tests for several hours, the high costs and the uncomfortable feeling of the patient when it comes to ambulatory urodynamics are perfect reasons to justify the choice of traditional urodynamics. The treatment should always be adjusted accordingly, with either increased medical therapy or more invasive treatment, and one thing is clear: ambulatory urodynamics and traditional urodynamics provide different results and should be used according to the physician's needs.
If you need urodynamics staffing assistance in your practice or hospital, click on the button below.

References
- Cameron AP. Incontinence: the role of ambulatory urodynamics in spinal cord injury. Nat Rev Urol. 2011;8(6):298-9.
- Bellucci CH, Wöllner J, Gregorini F, et al. Acute spinal cord injury--do ambulatory patients need urodynamic investigations?. J Urol. 2013;189(4):1369-73.
- Martens FM, Van kuppevelt HJ, Beekman JA, Heijnen IC, D'hauwers KW, Heesakkers JP. No primary role of ambulatory urodynamics for the management of spinal cord injury patients compared to conventional urodynamics. Neurourol Urodyn. 2010;29(8):1380-6.

