 Fecal incontinence (FI) is a common clinical condition with a negative impact on the quality of life. Commonly performed tests to evaluate fecal incontinence include anorectal manometry (ARM) and endoanal ultrasonography (EAU). In the following article, we will discuss this study, which aims to compare the results of these two tests in a cohort of patients with FI.
Fecal incontinence (FI) is a common clinical condition with a negative impact on the quality of life. Commonly performed tests to evaluate fecal incontinence include anorectal manometry (ARM) and endoanal ultrasonography (EAU). In the following article, we will discuss this study, which aims to compare the results of these two tests in a cohort of patients with FI.
Fecal incontinence is defined as the involuntary passage of stool in a person older than 4 years and for a period of 3 months or more. The prevalence is suspected to be more than 15%, with higher incidence in the geriatric age population.
FI: Main Causes
- Damage to anal sphincters secondary to obstetric or surgical trauma in the anorectal region
- Impaired rectal sensation related to diabetes mellitus or multiple sclerosis
- Decreased rectal compliance secondary to ulcerative colitis or radiation proctitis.
Patients with FI are evaluated with history, physical examination and endoscopy of distal colon and anal canal. The tests performed for the assessment of function and anatomy of the anal sphincter are:
- Anorectal Manometry (ARM) – sphincter physiology,
- Endoanal ultrasonography (EAU) – Sphincter Anatomy.
- Magnetic resonance imaging of the anal canal, electromyogram, and pudendal nerve terminal latency testing.
Aim of the Study
This study aims to compare the spectrum of ARM and EAU findings in a cohort of patients with FI who were being seen and evaluated in a gastrointestinal motility clinic setting with no initial goal of surgical repair and to determine the diagnostic contributions of both of these modalities.
Materials and Methods
ARM and EAU were performed on patients presenting with fecal incontinence. Colonoscopy and sigmoidoscopy of all patients were normal.
Protocol followed in all patients:
- Clinical data collection – demography, medical history, drugs, family.
- ARM - Polygram Net Software, water-perfused catheter was used for all ARM. Rectal sensation with intermittent balloon distension of rectum, resting pressure and maximal squeeze pressure were measured using station withdrawal technique.
- EAU – Single endoscopist evaluated all the patients, Defects of the EAS and the IAS were identified as disruptions to the fibrillar echo texture.
- Data analysis - To calculate the correlation between findings of ARM and EAU, linear regression analysis (Pearson’s correlation coefficient) was used. Measures analysed were the EAS and IAS function as measured by ARM and the sphincter morphology as gauged by EAU.
Results
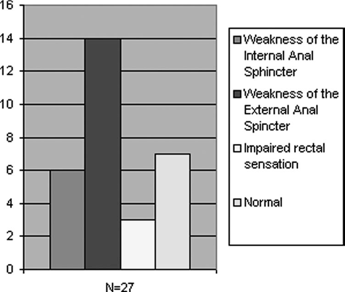
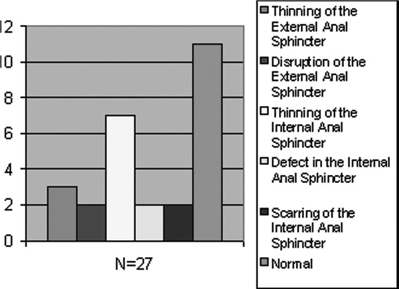
The following figures summarize the results obtained on ARM and EAU respectively:
Discussion
Results of our study indicate that the sphincter function assessed by ARM does not achieve a significant correlation with the sphincter morphology assessed by EAU in our cohort of patients referred to a gastroenterology clinic for evaluation of FI. However, EAU findings seem to correlate with ARM in cases of EAS thinning or partial or complete disruption of the sphincters. Results from previous studies seem to suggest that there is a very good correlation between these techniques in patients with partial or complete defects of the anal sphincter.
- Both men and women are at increasing risk of prevalence of FI even if it is due to varied etiologies.
- Thinning of anal sphincters on EAU was a commonly reported abnormality in the study. These sphincters have heterogeneously increased echogenicity on EAU and are thought to represent atrophic or degenerative sphincters, where there is replacement of the smooth muscle by fibrous tissue. They are not good candidates for surgery and must be managed non-surgically.
- On the basis of the results of this study, the researchers cannot recommend whether ARM or EAU is the better test for FI.
- However, our evidence indicates that both tests should be performed, because doing either test alone would have missed identifying abnormalities of the sphincters in up to one third of patients.
- Performing both the tests is appropriate and identifies patients who have more than one etiology for fecal incontinence, for example, those with a combination of sphincter defects and impaired rectal sensation.
- In centers without EAU facilities, a new procedure called the endoanal magnetic resonance imaging does provide visualization of the anal sphincter. Constraints with this technique include limited availability and higher costs.
Conclusion
In conclusion, patients with FI referred to a gastroenterology practice are middle aged and older patients of both sexes with varying etiologies. Although the yield of finding major sphincter defects was low, only a small percentage had normal EAU or ARM. When there is a partial or complete disruption of the anal sphincters, a good correlation with ARM is achieved. ARM and EAU are complimentary and important investigations for the thorough assessment of the anal sphincter apparatus, setting the stage for appropriate management strategies in the majority of patients with FI.


